Simplifying Provider Credentialing
NexCureMD offers fast, accurate, and fully compliant credentialing services. From document collection and CAQH profile management to payer enrollment and follow-ups, we handle everything so your practice can focus on providing excellent patient care without administrative delays or errors.

What We Offer
Our credentialing specialists manage your entire enrollment lifecycle, ensuring faster approvals and error-free submissions.
Provider Enrollment
Fast, accurate enrollment with insurance companies and government payers.
Re-Credentialing
Timely renewals to avoid disruptions in your reimbursement cycle.
CAQH Profile Management
Complete management and regular updates of your CAQH profile.
Professional Credentialing Services
NexCureMD simplifies the entire credentialing and enrollment process for healthcare providers. From document preparation to payer follow-ups, our team ensures smooth, error-free credentialing so you can focus on patient care while we handle the paperwork.
Our goal is to help practices get approved faster, avoid denials, and maintain compliance with federal and state regulations. Experience stress-free credentialing with our dedicated experts.
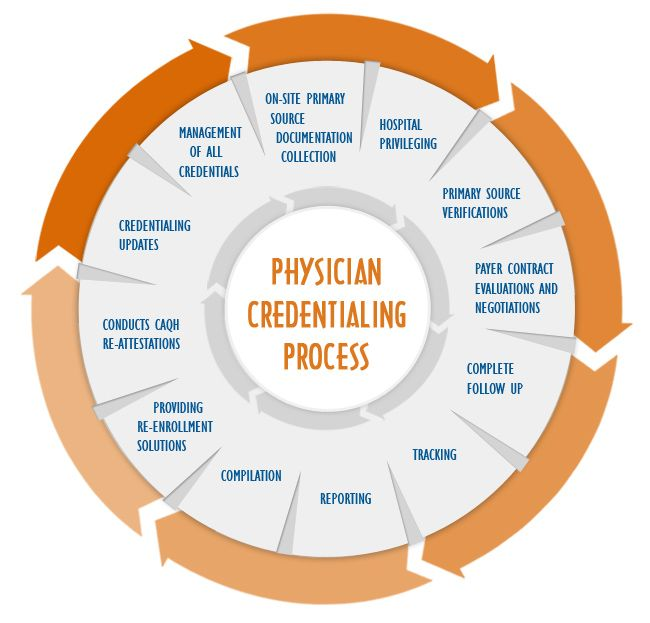
How Credentialing Works
A simplified process that eliminates delays and ensures smooth payer onboarding.
1. Provider Info Collection
2. Documentation Submission
3. Payer Application Filing
4. Follow-Up & Status Tracking
5. Approval & Activation
Why Credentialing Matters
Proper credentialing protects your practice, ensures compliance, and guarantees that you get paid for the services you deliver.
Stay Compliant
Avoid penalties and legal risks with fully compliant credentialing.
Faster Reimbursements
Approved providers get paid faster without claim rejections.
Build Patient Trust
Being credentialed increases transparency and patient confidence.
Your Credentialing, Our Responsibility
Let our experts handle complex forms, follow-ups, payer requirements, and compliance updates. You focus on your patients — we manage the rest.
Frequently Asked Questions
Answers to common questions about our credentialing services.