MIPS REPORTING AND CONSULTING SERVICES
Report to the highest payment incentive models with our MIPS consultants against your value-based healthcare services. Report to the highest payment incentive models with our MIPS consultants against your value-based healthcare services!

MIPS
MIPS helps healthcare practices enhance quality, boost reputation, and earn incentives while maintaining accountability. Eligible practices must participate to avoid penalties, though hardship exceptions exist for rural or underserved areas.
For 2025, the performance threshold is 75 points, with penalties capped at –9%. New specialty pathways (MVPs) and simplified reporting for small practices make participation easier than ever. Reporting remains open through March 31, 2026.
Ultimately, MIPS is about delivering value, improving care, and ensuring your practice thrives through quality and efficiency.
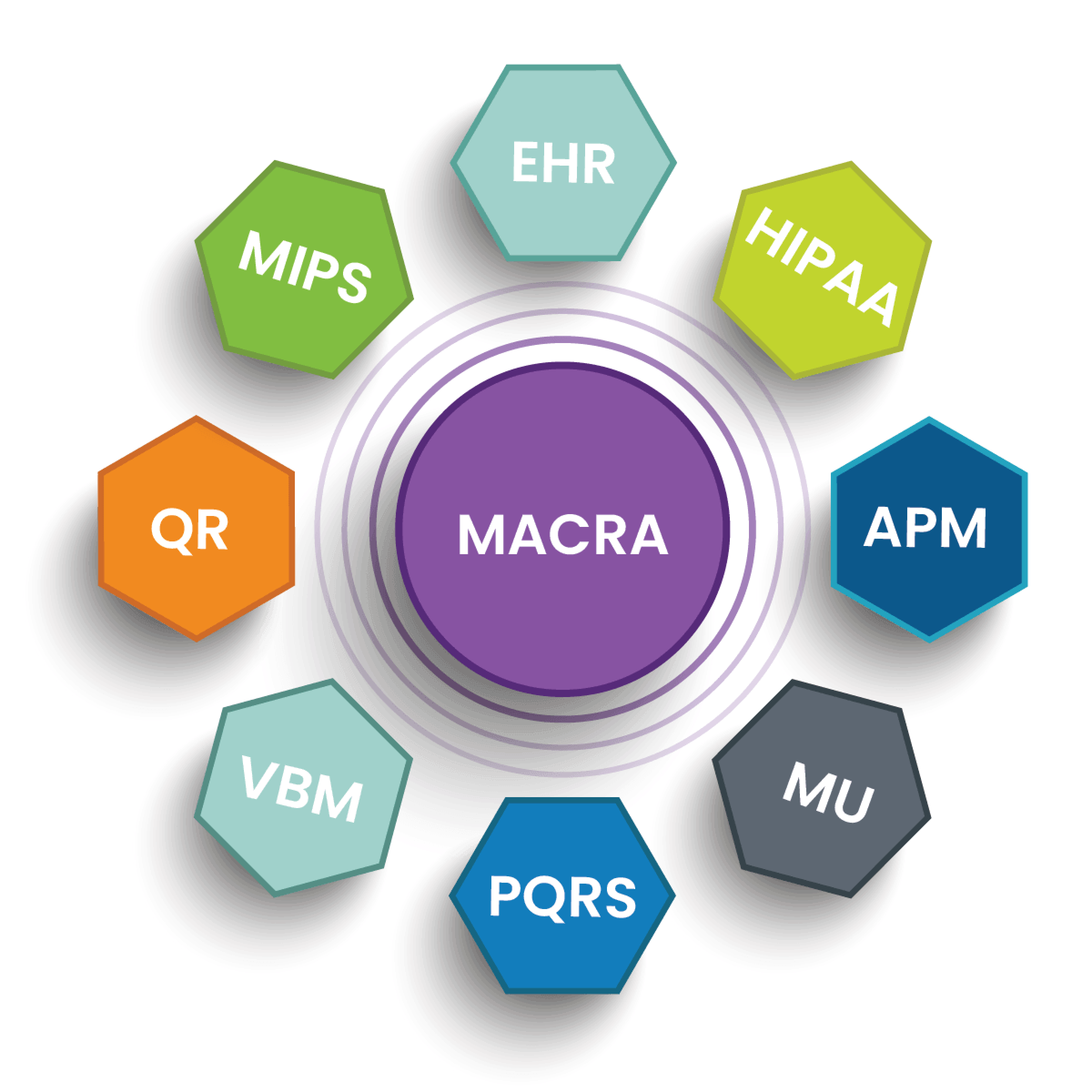
MIPS Categories
Quality
Replaces PQRS
Promoting Interoperability
Replaces MU
Improvement Activities
New Category
Cost
Replaces VBM
MIPS 2025 Important Highlights
- The Quality category is measured over the entire 2025 year.
- The Cost category accounts for 30% of the total MIPS score with no data submission required.
- Clinicians must complete Improvement Activities (IA) for a minimum of 90 consecutive days.
- Promoting Interoperability (PI) requires at least 180 consecutive days.
- The MIPS data submission deadline is March 31, 2026.
- CMS provides performance feedback to 2025 participating clinicians in 2026.
- MIPS payment adjustments begin on January 1, 2027.
MIPS Essential Steps
Follow these key steps to successfully navigate MIPS reporting and maximize your performance score.
1. Eligibility Check
2. Select Measures
3. Data Collection
4. Submit Data
5. Receive Score
QPP: Raising the Standard in Value-Based Healthcare
The Quality Payment Program (QPP) transforms Medicare from a volume-driven model to a value-based approach, fostering a healthcare environment that prioritizes patients, their well-being, and safety while leveraging advanced technology. A key component of this initiative is the MIPS reporting program.
QPP replaces the outdated SGR (Sustainable Growth Rate) formula with a modern Pay-for-Performance (P4P) framework. This shift allows CMS to streamline regulations and update legacy systems that previously added complexity without meaningful impact, helping clinicians focus on delivering high-quality care.
OUR NUMBER OF ACCOMPLISHMENTS
Evolving state-of-the-art billing strategies for all medical specialties fully compliant with HIPAA regulations and CMS Quality matrix.
93%
Exceptional Performance
100%
Clinicians Avoided Penalties
100%
HIPAA Compliance
Get Started with NexCure MD